Diabetic vs. Hypertensive Retinopathy
Diabetes and hypertension are among the most common diseases in developed countries, and unfortunately, the frequency of both diseases does increase with age. Because of this, both of these does have ocular complications, that may lead to blindness, if not monitored and controlled.
Diabetic retinopathy is a complication of diabetes mellitus and it can lead to blindness, if the DM is not under tight control. Risks of blindness increases the longer the disease process, how well you have it under control, and your blood pressure reading. There are two major types of diabetic retinopathy: nonproliferative and proliferative.
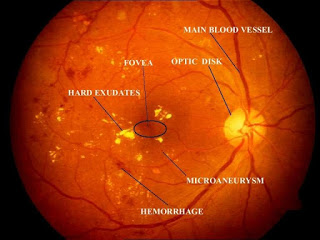
- Nonproliferative: This is the most common form of retinopathy and occurs when the capillaries in the back of the eye “balloons” and form pouches. Nonproliferative retinopathy is classified into three stages, depending on the severity of the damages.
- Mild Nonproliferative DR: Presence of a single small dot of bleeding in the back of the eye (micro aneurysms).
- Moderate Nonproliferative DR: Presence of multiple retinal hemorrhages.
- Severe Nonproliferative DR: Presence of new vessel and hard exudate formations.
- Proliferative: This occurs when the small blood vessels are so fragile and so damaged that they start to shut down, leading to a hypoxic environment; in other word, the retina is starved for oxygen! In response to this starvation, new blood vessels starts to grow into the retina. Unfortunately, these new vessels are very fragile, weak, and quite incompetent. This leads to them breaking apart very easily and ultimately leaking blood into the back of the eye, thus, blocking vision. Once this occurred, it’s called a vitreous hemorrhage. Secondly, the new fragile blood vessels can also cause scar tissue to proliferate. Then, after the scar tissue begin to shrink, it distort the retina and/or rip it out of place, thus, causing a retinal detachment to occur, ultimately leading to vision loss.
- *Macular Edema (Clinically Significant Macular Edema): The macula is one of the most important part of the eye, because it enables you to see fine details at distance and at near. Once it is compromise, either because of swelling and/or leaking of fluids into this space, vision loss can occur very rapidly and treatment must be initiated to reduce the swelling and/or leaking as soon as possible, to either preserve vision or to attempt to reverse any vision damages. Time is of the essence.
Diabetic retinopathy tend to occur the longer you’ve had diabetes. Thus, almost everyone with type 1 diabetes, and most with type 2 diabetes, likely have some form of nonproliferative diabetic retinopathy. Proliferative retinopathy, on the other hand, is somewhat less common, however, it does have a much more damaging effect once occurred. Because your retina can be severely damaged before any change in vision is noticed, it is highly recommended that diabetic eye exams are performed on an annual basis.
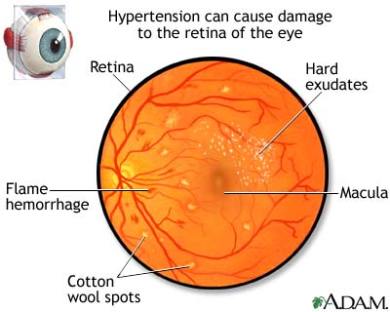
Hypertensive retinopathy is a condition in which there are changes in the retina due to high blood pressure. In a normal eye, the retinal arteries are able to hold their own shape even if there are changes in systemic blood pressure. However when this pressure exceeds 140/110 mmHg, they are unable to control it. This can have serious affect on the retina. Hypertensive retinopathy can affect any age and anyone who have had uncontrolled high blood pressure. This high pressure dynamic causes a change in the retinal blood vessels by:
- Causing blood vessels to become narrow and makes arteries and veins to cross over, on top of each other.
- When the blood vessels change its original shape, they can leak blood and fluid easily. This leaking can cause swelling of the optic nerve, as well as the macula.
- When retina is detached, other nearby areas can become swollen.
- Grade 1: Very mild narrowing of the retinal arteries.
- Grade 2: More severe and tighter constrictions/compression of the retinal arteries, leading to a condition called arteriovenous (AV) nipping.
- Grade 3: More severe than Grade 2, with retinal edema, micro aneurysms, cotton wool spots, and retinal hemorrhages.
- Grade 4: More severe than Grade 3, with secondary optic disc and/or macular edema. Once Grade 4 is noted, patients tend to have a much higher risk for stroke and/or kidney or heart disease.